Nowadays, diabetes and kidney disease have attracted much attention. The incidence of diabetes continues to rise, and kidney disease also threatens human health. When the two meet, it brings great challenges to patients. It is important to have a deep understanding of their relationship. This article will explore their basic cognition, mutual relationship, treatment and prevention measures.
Basic knowledge of diabetes and kidney disease
Common types of diabetes
Type 1 diabetes usually develops during adolescence and is caused by the destruction of pancreatic β cells, leading to absolute insulin deficiency.
Type 2 diabetes is common in middle-aged and elderly people. It is closely related to lifestyle, genetics and other factors, and is often manifested as insulin resistance and relative insulin deficiency.
Gestational diabetes occurs during pregnancy and is related to hormonal changes during pregnancy.
A special type of diabetes caused by specific gene mutations, endocrine diseases or drugs.
Common types of kidney disease
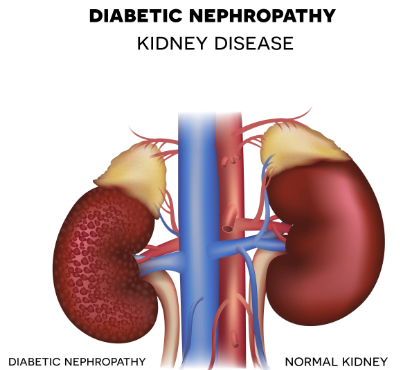
Kidney diseases mainly include acute glomerulonephritis, rapidly progressive glomerulonephritis, IgA nephropathy, nephrotic syndrome, chronic glomerulonephritis, etc. It also includes secondary kidney diseases such as diabetic nephropathy, hypertensive nephropathy, etc.
The relationship between diabetes and kidney disease
Mechanism of diabetes-induced kidney disease
Diabetes mellitus can induce kidney disease through multiple mechanisms.
First, long-term hyperglycemia leads to abnormal local glucose metabolism in the kidneys, which increases the amount of glucose metabolized by the kidneys and increases the glucose load on the kidneys.
Secondly, glomerular hyperperfusion, high transmembrane pressure and high filtration state play a key role in the occurrence of diabetic nephropathy.
Furthermore, oxidative stress causes excessive production of reactive oxygen species, while the body’s antioxidant capacity decreases, affecting kidney function.
In addition, immune-inflammatory factors, such as the complex interactions of the complement system and pattern recognition receptors, and the involvement of various inflammatory factors, increase the risk of kidney disease.
Finally, genetic factors also play an important role in susceptibility to diabetic nephropathy.
The adverse effects of kidney disease on diabetes
Kidney disease can adversely affect blood sugar control and the progression of diabetes in people with diabetes.
On the one hand, the kidneys are organs that process waste in the body, and impaired function may affect the metabolism and excretion of insulin, leading to increased blood sugar.
On the other hand, kidney disease can affect the body’s water and salt metabolism, causing edema and weight gain, thereby increasing the risk of diabetes.
At the same time, kidney disease affects the body’s metabolism and hormone secretion, thereby affecting the release and action of insulin, leading to the occurrence and aggravation of diabetes.
Treatment of diabetic kidney disease
Drug treatment
Drug treatment for diabetic nephropathy mainly includes drugs to control blood sugar, blood pressure and proteinuria.
Common drugs for controlling blood sugar include biguanides (such as metformin), sulfonylureas (such as glimepiride), glinides (such as nateglinide), thiazolidinediones (such as rosiglitazone), α-glucosidase inhibitors (such as acarbose), etc.
Non-drug treatment
Dietary control is crucial for patients with diabetic nephropathy.
Diet: Reduce the intake of plant protein and consume appropriate amounts of high-quality protein such as fish, eggs, and milk.
Exercise: You can choose a moderate amount of aerobic exercise, such as brisk walking, jogging, etc., which will help to strengthen your physical fitness, control your weight, and improve your blood sugar and blood pressure levels.
Psychological adjustment: Maintaining a positive and optimistic attitude and building confidence in overcoming the disease will help stabilize and recover from the disease.
Preventive measures for diabetic nephropathy
Prevention in daily life
A regular schedule is essential for the proper functioning of the body.
Adequate sleep helps maintain the body’s metabolic balance, enhance immunity and reduce the risk of disease.
At the same time, quitting smoking and limiting alcohol consumption are also important measures to prevent diabetic nephropathy.
Smoking can damage vascular endothelial cells, affect blood circulation, and increase the burden on the kidneys; excessive drinking may cause blood sugar fluctuations and increase the risk of diabetes.
In addition, maintaining moderate exercise, such as 30 minutes of brisk walking, swimming and other aerobic exercises every day, can promote metabolism, control weight, enhance cardiopulmonary function, and help maintain a healthy body.
Regular physical examination and monitoring
Regular blood sugar, kidney function and other related tests are very necessary to prevent diabetic nephropathy.
For diabetic patients, it is recommended to test glycosylated hemoglobin every 3-6 months to understand the control of blood sugar.
Renal function tests should be performed at least once a year, including testing of blood creatinine, urea nitrogen, glomerular filtration rate and other indicators.
